Horner's syndrome
- Dr Andrew Matole, BVetMed, MSc

- Jul 23, 2023
- 10 min read
Updated: Jul 25, 2023
What is a syndrome?

A syndrome is a term given to a group or set of signs, symptoms or conditions that when they occur together they significantly suggest the presence of a certain disease or an increased chance of developing the disease. The presence of a syndrome does not mean it is a diagnosis. However, since a syndrome often has a limited number of causes, the recognition of a specific syndrome allows one to narrow down to a small number of possible disease causes (ie the diagnosis).
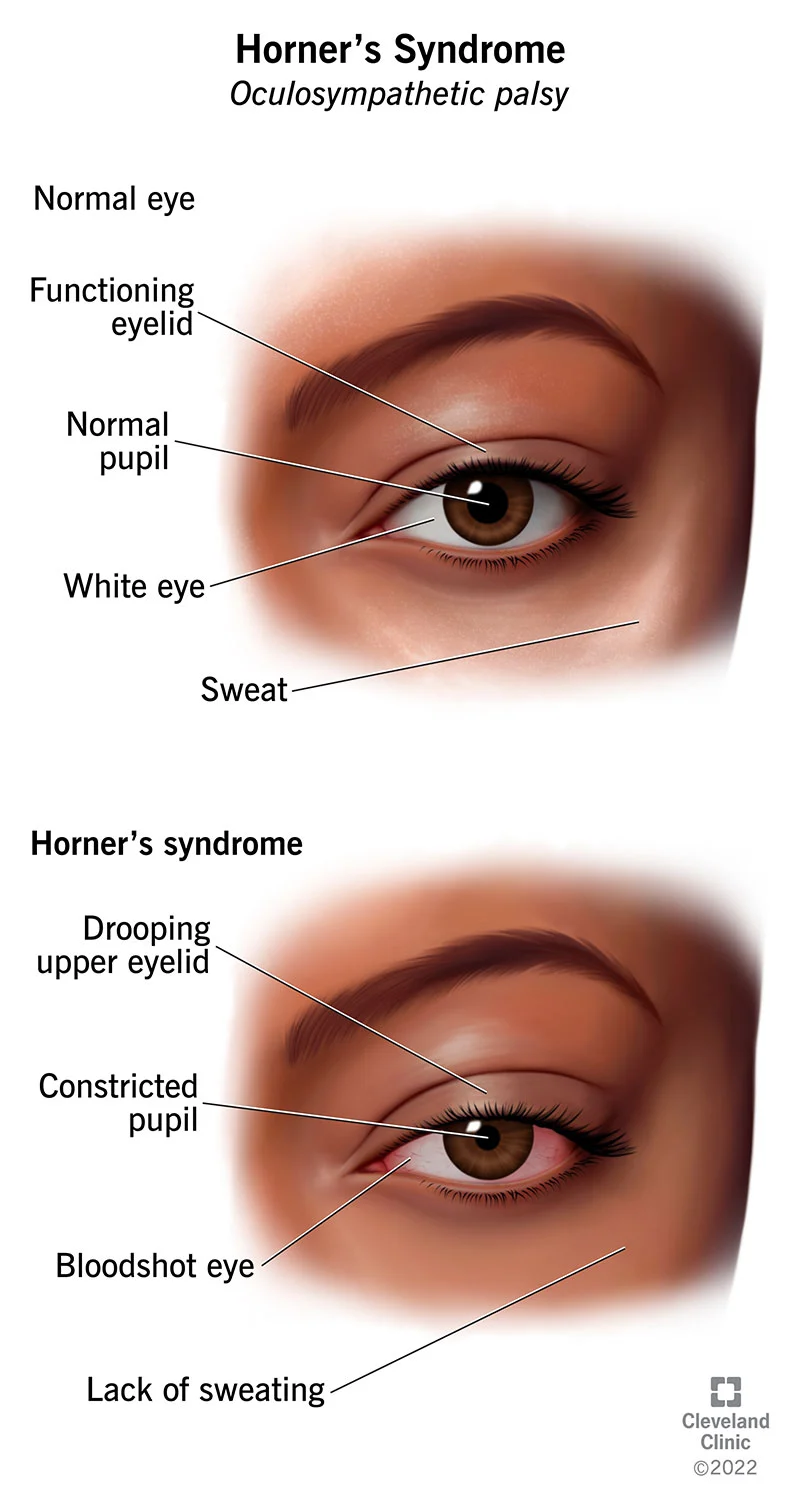
Horner's syndrome, therefore, is a collection of signs resulting in a constricted, small pupil (miosis); drooping of the upper eyelid; a slightly sunken eyeball in the eye socket (enophthalmos) and protrusion of the third eyelid. Damage to the sympathetic nervous system, which supplies the eye on the affected side of the head, is what causes the disorder. It happens in both animals and humans.
What is the sympathetic nervous system?
The nervous system regulates a wide range of bodily functions; however they are utterly unnoticed. The neurological system automatically controls and regulates the heart and respiratory rates, sweating, blood circulation to various body parts, pupil dilation, and constriction. The autonomic nervous system, thus, refers to the portion of the nervous system that controls these automatic systems and is divided into two subtypes, the sympathetic nervous system and the parasympathetic nervous system. The sympathetic nervous system gets the body ready for a "fight or flight" scenario whereas the parasympathetic nervous system keeps things as they are, facilitating "rest and digest." The sympathetic nervous system may cause several changes, such as an increase in sweating, dilated pupils, a faster heartbeat, and an increase in blood flow to the muscles. The healthy body coexists with both systems in harmony.

The sympathetic nerve fibers in the eye broaden the eyelids, lower the third eyelid, and hold the eye forward in the socket. They also enlarge the pupil. For protection, the parasympathetic nerves narrow the pupil, elevate the third eyelid, and retract the eye. Both systems are usually active at the same time, with one system occasionally outperforming the other depending on the situation. Only the parasympathetic nerves function when the sympathetic nerves controlling one of the eyes are injured, and then Horner’s syndrome results.
Why do dogs suffer Horner's syndrome?
Neurons are little nerve fibers that carry the sympathetic nerve supply to the eye. Horner’s syndrome is brought on by injury to any section of this lengthy nerve, which is a three-neuron pathway. In addition, certain parts of the pathway are more likely to have injuries than others. Therefore, the diagnosis is made easier by knowing where along the pathway the problem is likely to be.

Which nerves supply the eye muscles?
The eyelid muscles are innervated by three out of the twelve cranial nerves. These are the cranial nerve III (the oculomotor nerve), cranial nerve V (the trigeminal nerve), cranial nerve VII (the facial nerve), and sympathetic nerve fibers.
Cranial nerve III (the oculomotor nerve) innervates the main upper eyelid muscles causing lower eyelid retraction in downgaze. The oculomotor nerve also carries parasympathetic fibers that supply the intrinsic muscles of the eye and transmits propriosensation from the extraocular muscles.
Cranial nerve V (the trigeminal nerve) supplies the upper eyelid and the medial aspect of both upper and lower lids, with sensation to the eyelids being supplied by the terminal branches of the ophthalmic (V1) and maxillary (V2) divisions of the nerve, the trigeminal nerve. The cell bodies of the terminal branches originate in the trigeminal ganglion.
The ophthalmic (V1) division divides further into the lacrimal, frontal, and nasociliary nerves. The lacrimal nerve terminates in the lacrimal gland, but also innervates the conjunctiva and lateral upper eyelid skin. The frontal nerve innervates the conjunctiva, the skin of the upper eyelid and supplies additional sensation to the forehead and scalp. The nasociliary nerve supplies the medial structures of the external eye, including the medial conjunctiva, lacrimal sac, and medial upper and lower eyelids.
The facial nerve (CNVII) innervates the eyelid muscles and supports eyelid protraction. Sympathetic fibers contribute to both upper and lower eyelids retraction.

The maxillary division (V2) supplys the lower eyelid, the conjunctiva, the skin of the lateral temple, and the lateral cheek.
Cranial nerve VII (the facial nerve), divides into the temporal, zygomatic, and buccal branches and supply the muscles of the face and the eyelids.

The Sympathetic nerve pathway to the eyelid muscles originates in the hypothalamus within the brain, the neuron then exits the brain travels through the brainstem and synapse in the spinal cord. This is referred to as the core or central neuron or first order neurons.

The Second-order neuron in the pathway then synapses (connects) with the first-order neuron, exits the spinal cord, enters the chest at the beginning of the neck, between the first, second, and third thoracic vertebrae, subsequently develops the cervical sympathetic trunk, a network of nerves that ascends the neck once more to the area of the middle ear without passing through the spinal cord this time. The pre-ganglionic neuron or second order neuron is the name of this section and it synapses in the superior cervical ganglion with the Third-order neuron.
The Third-order neuron then travels along the carotid artery to the ophthalmic division of the trigeminal and enter the orbit. The third order neuron, also referred to as the postganglionic neuron, is the final nerve segment and this section extends all the way from just below the ear to the eye.
A diagrammatic representation of the three-neuron sympathetic pathway: (a) normal - source: www.veteriankey.com; (b) disrupted in Horner's Syndrome - source: lubner, et al.
Damage to any part of this pathway can result in Horner's Syndrome.
Pathological changes at any one of these several sites lead to failure of sympathetic nerve supply to the eye and the surrounding structures causing loss of smooth muscle tone and hence the clinical signs.

Horner’s syndrome, therefore, may develop in the neck, spinal cord, chest, neck, ear, or eye regions. Damage from trauma, the existence of a tumor, an infarction (abnormal blood clot), an ear infection, or disorders of the eye itself can all lead to the condition. Knowing which segment is implicated helps us determine what caused the injury because each segment of the nerve pathway is susceptible to different kinds of harm.
Which breeds are predisposed to Horner's Syndrome?
Horner's syndrome is more predisposed in middle age companion animals with the dog breeds most affected being the Golden Retriever, Bearded Collie, Rough Collie and Smooth Collie. Dogs with a proclivity to develop spinal cord and middle ear disease are more at risk.
What clinical signs do dogs show?
Idiopathic Horner’s syndrome is the most common form observed in dogs, about half of the cases, meaning it has an no known cause. In cats, however, idiopathic Horner's syndrome is very rare as a cause is always found, with many cats that develop the syndrome having a recent history of trauma. The possible lesions occur anywhere along the sympathetic pathway to the eye, i.e., the brainstem, cervical spinal cord, T1-T3 spinal cord, brachial plexus, intrathoracic, vagosympathetic trunk, middle ear, or the retrobular.
Dogs frequently display the following symptoms:
1. Ptosis, whereby the upper eyelid droops.
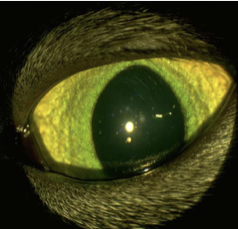
2. Miosis, whereby the pupil constricts (the affected pupil becomes smaller than the unaffected pupil).

3. Enophthalmos, whereby the eyeball is slightly sunken into the eye socket (occurs due to loss of innervation of the muscles in the orbit making them relax, sinking the eye).
4. Third eyelid protrusion (occurs passively due to the enophthalmos described above).
5. Hyperemia of the conjunctiva (reddening of the white of the eye, e.g., due to uveitis).

6. Ear problems associated with middle ear disease. Ipsilateral ear may feel warm due to local vasodilation.

7. Forelimb lameness due to involvement of cervical intumescence (swelling) and brachial plexus injury by root avulsion or loss of panniculus reflex on same side with brachial plexus pathology.

8. Drooping of facial muscles.
9. Following jugular blood sampling if vagosympathetic trunk is damaged.
10. Trauma to neck area, e.g., bite or surgery to the neck causing severe cervical cord injury.

11. Dyspnea or dull percussion to chest if significant thoracic mass or mediastinal pathology is present.
First order Horner's syndrome is almost always accompanied by severe neurological abnormalities that are usually linked to lesions of the midbrain, brainstem, or cervical spinal cord. Occasionally, only two or three of the signs may be present and this is referred to as Partial Horner’s syndrome.
How is Horner's Syndrome diagnosed?
Ideally, the dog needs to go through a neurological examination to see if there are any other signs that indicate where in the sympathetic nervous system the problem is likely to be. There are several tests that can be done to diagnose Horner's Syndrome and include:-
1. Pharmacological Testing
This test is done using Phenylephrine. It can also be referred to as Phenylephrine test. Phenylephrine is a direct acting sympathomimetic drug, and is administered to both eyes and time it takes for the pupils to dilate is noted.
The test is based on the principle of denervation hypersensitivity of the iris dilator muscle increasing their sensitivity to direct-acting sympathomimetics following denervation. This phenomenon usually takes up to 2 weeks to develop.
Topical 1% phenylephrine (1 drop) is used to assess level of lesion and resolution of signs within a given time period indicates where the lesion is:
At 20 min, resolution of clinical signs implies third order disease as seen with idiopathic Horner syndrome.
At 40 min, resolution of clinical signs implies second order disease.
At 60-90 min, resolution or no change of signs implies first order disease.
2. Radiography
Thoracic radiographs when done can help to identify thoracic/mediastinal masses interfering with nerve conduction.

3. Others
Cerebrospinal fluid (CSF) tap or sampling to look for spinal cord and brain disease.
Electromyography to test for brachial plexus avulsion or tumor.
CT/MRI to examine brain, middle ear and cervical spinal cord.
Horner's syndrome, therefore, is caused by the disruption at some point along the oculosympathethic pathway from the hypothalamus to the eye, resulting in the classic triad clinical features of miosis, ptosis, and anhydrosis. Since the oculosympathetic pathway has a long course, there is the potential for involvement by many different disease processes. However, given that some are potentially life-threatening such as internal carotid aneurysms and malignancies, it is important to have a systematic approach to diagnosis and management.
What diseases affect the first order neuron?

The most unusual site for Horner's syndrome is the first part of the three-neuron pathway. Most conditions that cause first order symptoms of the Horner's syndrome itself also cause other symptoms that are more worrisome. The causes in this part include:-
Tumors in the hypothalamus,
Vascular illnesses (like a stroke),
Fibrocartilaginous embolism in the spinal cord (where a small piece of intervertebral disc material blocks a small spinal vessel),
A herniated intervertebral disk in the neck region
A sudden interruption of the blood flow to the brainstem.
Spinal cord injury.
Multiple sclerosis (MS).
Chiari malformation whereby the lower part of the cerebellum – the “tonsil” – is forced downward into the spinal canal.
Encephalitis.
Meningitis.
Lateral medullary syndrome (Wallenberg syndrome).
Syringomyelia.
All the above are diseases that affect nerve fibers in the brain, brainstem, or spinal cord. Any one of these can result in Horner's syndrome and further neurological problems, such as lameness, limb weakness or wobbliness, aberrant awareness, or pain. An MRI or other form of advanced imaging may be recommended. If the cause of the Horner's syndrome emanates from the first part of the three-neuron pathway, the syndrome is referred to as First-order (central) Horner's syndrome.
What diseases affect the second order neuron?
The second-order neuron is affected by or damaged by any of the following:-
Tumors in the upper part of the lungs or chest cavity.
Trauma to the neck or chest cavity due to a surgery or accident.
Brachial plexus injury.
An abscessed tooth in the jaws.
Forelimb injuries, particularly after trauma of the leg caused by pulling, can cause the nerves that exit the spinal cord in the armpit area to be overstretched, damaging the cervical sympathetic trunk.
Horner's syndrome can also develop weeks or months after an initial forelimb lameness that was caused by a tumor of the brachial plexus that is progressively enlarging in these nerves.

7. The sympathetic trunk can occasionally be harmed by a mass in the chest (in the area known as the cranial mediastinum), such as a tumor.
8. A second order lesion could be caused by neck trauma that is severe enough, such as tugging very firmly on a lead.
If the cause of the Horner's syndrome emanates from the second part of the three-neuron pathway, the syndrome is referred to as Second-order (pre-ganglionic) Horner's syndrome.
What diseases affect the third order neuron?
These are the most significant causes of Horner's syndrome, and they include: -

Lesions on the carotid artery.
Middle ear infections.
Injury to the base of the skull.
Raeder paratrigeminal syndrome.
Internal carotid artery dissection or a carotid artery aneurysm.
Shingles (herpes zoster).
Temporal arteritis.
Idiopathic Horner's syndrome and ear diseases are the most prevalent.
Horner's syndrome is a condition that is readily caused by middle ear inflammation. Middle ear infections can occasionally be linked to vestibular dysfunction (which manifests as a head tilt, balance problems, and irregular eye flicking, or nystagmus), as well as weakness or paralysis of the face on the Horner's syndrome side. Idiopathic conditions, however, are a final and frequent cause of Horner's syndrome. This phrase suggests that although we do not understand the underlying reason, the issue usually goes away on its own after an average of 8 weeks (but it may take up to several months) without having any negative long-term impacts. Therefore, this is the most likely diagnosis if the aforementioned investigations come up clean. If the cause of the Horner's syndrome emanates from the third part of the three-neuron pathway, the syndrome is referred to as Third-order (post-ganglionic) Horner's syndrome.
How Horner's syndrome treated?
It is not necessary to treat Horner's syndrome. The syndrome is not painful and does not interfere with vision. The significance of the syndrome is that it indicates nerve damage that must be recognized. For cosmetic reasons, phenylephrine eye drops can be prescribed to relieve clinical signs. The most important thing is to determine what caused the Horner's syndrome. The Horner's syndrome itself probably does not need treatment, but its underlying cause very well might. Therefore treatment is aimed at management/treatment of the underlying cause/s of the disease and supportive care. As such, advanced imaging, including MRI is imperative to ascertain if middle ear disease or another disease process (tumor etc) is the underlying cause, and to decide on the most appropriate treatment, ie surgery on the middle ear, drainage options or medical management.
Topical sympathomimetics (2.5% phenylephrine, 1 drop TID) can transiently reduce conjunctivitis and nictitans membrane (third eyelid) prominence.
References
Boydell I P (1998) Horner's syndrome in a puppy. JSAP 39 (9), 448-9
Boydell P & Brogan N (2000) Horner's syndrome associated with Neospora infection. JSAP 41 (12), 571-572.
Boydell P (2000) Idiopathic Horner syndrome in the golden retriever. J Neuroophthalmol 20, 288-290.
Dutton, Jonathan J. Clinical Anatomy of the Eyelids. Ophthalmology. By Myron Yanoff and Jay S. Duker . Elsevier Inc, 2013. 4th ed. 1255-1257.e1
Gelatt K N (1999)Veterinary ophthalmology.3rd Edn. Williams & Wilkins.
Gao, Zoe MBBS; Crompton, John L. MBBS, FRANZCO, FRACS. Horner Syndrome: A Practical Approach to Investigation and Management. Asia-Pacific Journal of Ophthalmology 1(3):p 175-179, May/June 2012. | DOI: 10.1097/APO.0b013e318256009d
Garosi L, Lowrie M (2014) Neuro-ophthalmology. In: BSAVA Manual of Ophthalmology. 3rd edn. Gould D & McLellan G (eds). BSAVA.
Harris, Paul and Bryan Mendelson. Eyelid and Midcheek Anatomy. Putterman's Cosmetic Oculoplastic Surgery. Elsevier Inc., 2008. p45-63.
Lubner, R., Fridley, J., Choi, D., Telfeian, A., Cahill, J., Gokaslan, Z., Oyelese, A. Cervical myelopathy presenting with an acute Horner's syndrome,17. 10.1016/j.inat.2019.01.016
Journal Of Interdisciplinary Neurosurgery
Lin, Lily Koo. Eyelid Anatomy and Function. Ocular Surface Disease: Cornea, Conjunctiva and Tear Film. By Edward Holland, Mark Mannis, and W. Barry Lee. Elsevier Inc., 2013. p11-15.
Simpson K M, Williams D L, Cherubini G B (2015) Neuropharmacological lesion localisation in idiopathic Horner's syndrome in Golden retrievers and dogs of other breeds. Vet Ophthamol 18, 1-5.
Spivak R E, Elkins A D, Moore G E et al (2013) Postoperative complications following TECA-LBO in the dog and cat. JAAHA 49, 160-168.
"Orbital Nerves." Atlas of Clinical and Surgical Orbital Anatomy. By Jonathan J. Dutton. Elsevier Inc., 2011. 2ed. p51-82.





































Comments