Cellulitis in Pets (Dogs and Cats): Causes, Warning Signs, Diagnosis, Treatment, and Prevention
- Dr Andrew Matole, BVetMed, MSc

- Jan 11
- 10 min read
Introduction

Cellulitis is an acute bacterial infection of the deep dermis and subcutaneous tissue in both humans and companion animals. It is a painful, spreading inflammation of the tissues under the skin (the subcutis). The most common causative agents in humans are Streptococcus species and Staphylococcus aureus, while in pets, the most frequent species is Staphylococcus pseudointermedius, which is rarely pathogenic to humans (Bannoehr & Guardabassi, 2012; Ruiz-Ripa et al., 2021). The infection is most commonly caused by bacteria that penetrate a break in the skin barrier, such as a cut, bite, or other wound—sometimes a tiny puncture wound you cannot see. Because cellulitis can progress quickly and may spread along tissue planes, it should be treated as a time-sensitive condition (Johnson, 2023).

What exactly is cellulitis in companion animals?

In veterinary medicine, "cellulitis" usually refers to a widespread infection and inflammation of deeper skin and subcutaneous tissues, often with swelling, heat, pain, and sometimes fever, typically around bite or scratch wounds. Unlike a small, well-contained abscess, cellulitis can be more spread out and may not have a single obvious pocket of pus early on (Johnson, 2023).
Cellulitis may occur anywhere, but common “hot spots” include:
Limbs and paws (especially after thorn/grass penetration or small wounds)
Face/muzzle (from bites, scratches, foreign bodies, or dental-related spread in some cases)
The periocular/orbital area, which is behind or around the eye, can experience severe pain (Hamor, 2024).
What causes cellulitis in dogs and cats?
1) Skin breaks and wound contamination

Most bacterial cellulitis begins when bacteria enter through:
Bite wounds or scratches (including cat bites, which can seal over and trap infection)
Small lacerations, punctures, or torn nails
Surgical incisions (less common, but possible)
Pressure sores or chronic skin disease that disrupts the skin barrier
2) Foreign bodies (thorns, grass awns, splinters)

A penetrating foreign body can introduce bacteria and create a continuing inflammatory focus. The result is often recurrent swelling, draining tracts, or a cellulitis that does not fully resolve until the foreign material is removed.
3) Spread from nearby infections

Some cellulitis cases arise when infection tracks from adjacent structures; for example, infection/inflammation around the eye may spread from nearby sources or foreign bodies and can cause marked pain and swelling (Hamor, 2024)
4) The bacteria involved (why Staphylococcus matters)

In dogs, Staphylococcus pseudintermedius is a major bacterial pathogen associated with skin infections (including deeper infections that can resemble cellulitis). A key practical implication is that antimicrobial resistance—including methicillin-resistant strains—can complicate treatment and make effective diagnostics (cytology/culture) more important in non-responding or recurrent cases (Lynch, 2021; Roberts, 2024). While most staphylococcal infections in pets are caused by S. pseudointermedius, humans can transfer human-associated S. aureus strains to their pets, which can become carriers and a potential public health risk (Haag et al., 2014; O'Shea et al., 2016).
What are the major types of cellulitis in pets?
In veterinary medicine, cellulitis is largely classified by anatomical location, because different regions have different complications and levels of urgency.
1. Periocular (Periorbital) Cellulitis

Periocular cellulitis affects the eyelids and skin surrounding the eye. In dogs and cats, it commonly develops after:
Thorn or grass-seed penetration
Bite wounds near the face
Spread from nasal, oral, or sinus infections
Affected animals develop facial swelling, eyelid redness, squinting, and pain. Unlike in human children, periocular cellulitis in animals frequently progresses to deeper orbital involvement if not treated promptly (Hamor, 2024).
In veterinary patients, facial swelling should always be treated as potentially serious due to the close anatomical connections among the skin, sinuses, and the eye orbit (Hamor, 2024).
2. Orbital Cellulitis
Orbital cellulitis is a medical emergency. It involves infection of the fat and muscles behind the eye, often arising from:
Penetrating foreign bodies (sticks, thorns)
Severe facial wounds
Dental root infections
Deep bite wounds

Clinical signs include:
Bulging of the eye (exophthalmos)
Severe pain when opening the mouth
Fever and lethargy
Vision loss in advanced cases
Without rapid treatment, orbital cellulitis can lead to blindness or brain infection (Hamor, 2024; Maggs et al., 2018).
3. Facial Cellulitis
Facial cellulitis is common in dogs and cats, following:
Cat or dog bites
Tooth root abscesses
Sinus or nasal infections
Insect or spider bites
Penetrating foreign material
It causes rapid facial swelling, heat, pain, and skin tightness. Because facial tissues drain toward the eyes and brain, facial cellulitis is always treated aggressively in veterinary medicine (Miller et al., 2013).
4. Limb and Paw Cellulitis (Most Common)

One of the most frequent presentations is paw or leg swelling after thorn or grass-seed penetration. Dogs often develop cellulitis in:
Paws
Toes
Lower legs
This occurs when bacteria are introduced deep into the tissue through a tiny puncture wound. Clinical signs include limping, painful swelling, heat, and reluctance to bear weight (Johnson, 2023). Foreign bodies frequently remain hidden, leading to recurrent cellulitis or abscesses until they are removed (Miller et al., 2013).
5. Bite-Associated Cellulitis (Especially in Cats)

Cat bites are a leading cause of cellulitis because their sharp teeth inject bacteria deep into the tissues, while the skin closes quickly over the wound. These infections are commonly caused by Pasteurella multocida and Staphylococcus species (Johnson, 2023).
Signs appear within 24–72 hours and include:
Local swelling
Heat and pain
Fever
Abscess formation or diffuse cellulitis
Without treatment, the infection can spread rapidly.
6. Truncal (Body Wall) Cellulitis

Cellulitis can also affect the chest, abdomen, or neck, following:
Bite wounds
Surgical complications
Injection site contamination
Skin trauma
This form often causes large areas of firm, painful swelling and systemic illness.
Why does cellulitis spread in pets?
In dogs and cats, the loose connective tissue beneath the skin allows bacteria to spread quickly over large areas, unlike in humans, where infections are more localised. This is why veterinary cellulitis often looks dramatic and spreads rapidly (Miller et al., 2013).
What are the clinical signs of cellulitis in pets?
Cellulitis can look different depending on location and severity. Common signs include:
Local signs
Swelling that may expand over hours to days
Heat and marked pain when touched
Redness may be present, but in thick-coated pets it can be hard to see
Skin may feel tight; the pet may limp if a limb is involved
Possible oozing, draining tracts, or a soft fluctuant area if an abscess forms
Whole-body signs (more concerning)
Fever, lethargy, reduced appetite
Shivering, reluctance to move
In severe cases, rapid progression of swelling and pain
Eye/orbit red flags (urgent)
If infection involves tissues around/behind the eye, you may see:
Swelling around the eye, squinting, tearing
Pain on opening the mouth (a classic clue in dogs)
Bulging eye (exophthalmos) or third eyelid elevation.
These signs warrant same-day assessment (Hamor, 2024).
Other general symptoms
The other general symptoms include:
Sensitivity and pain
Redness, swelling, and skin that is hot to the touch
Abscess formation with potential pus or green discharge
Obsessive licking of the affected area
Systemic signs like fever, lethargy, or loss of appetite.
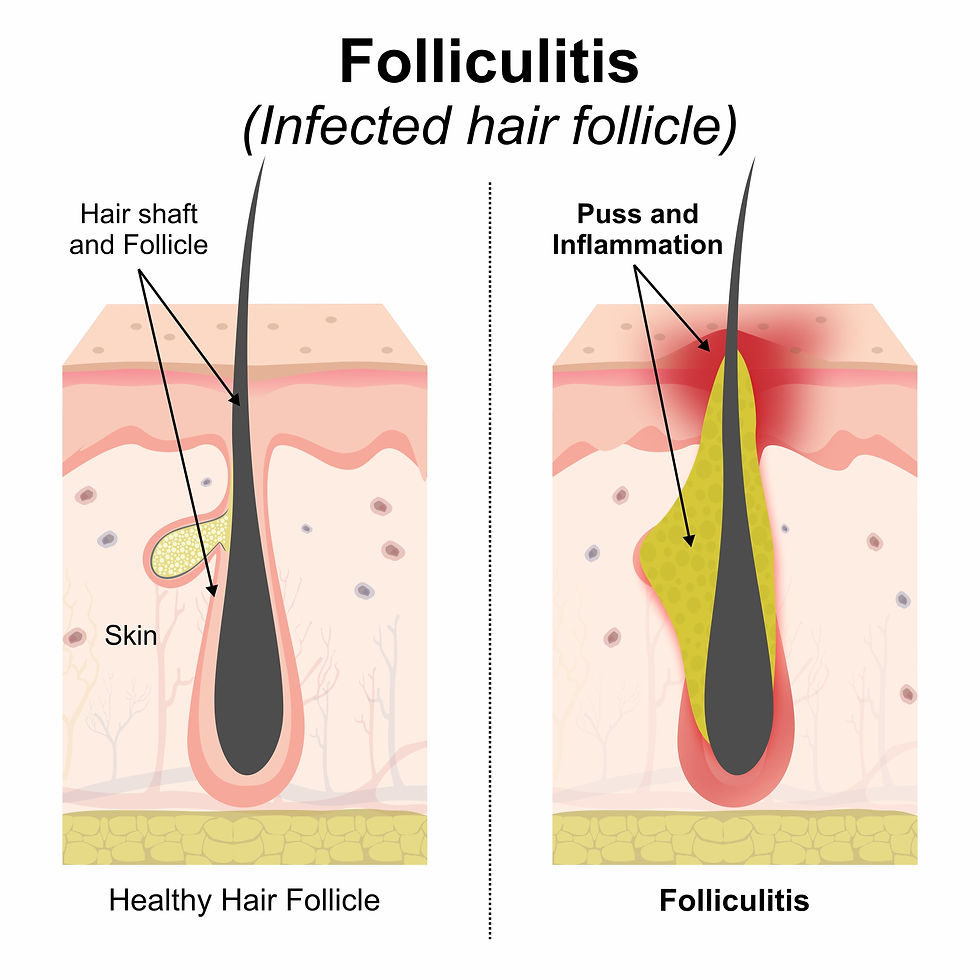
Cellulitis, abscess, & “hot spots” (the distinction)
In companion animal medicine, cellulitis, abscesses, and hot spots represent distinct forms of skin and soft-tissue disease that differ in depth, spread, and clinical management. Cellulitis is a diffuse bacterial infection of the deep dermis and subcutaneous tissues that spreads along connective tissue planes, producing painful swelling, heat, and often systemic illnesses without forming a localised pocket of pus (Johnson, 2023; Miller, Griffin, & Campbell, 2013). An abscess, on the other hand, is a localised, encapsulated collection of pus that forms when the immune system blocks off infection. This situation happens most often after a bite wound, especially in cats (Miller et al., 2013). Hot spots (acute moist dermatitis) are superficial, self-trauma–induced inflammatory lesions driven by itching and moisture, in which bacterial overgrowth is limited to the skin surface and does not involve deep tissues, making them biologically and therapeutically distinct from cellulitis and abscesses (Loeffler et al., 2025; Miller et al., 2013). Pet owners often use "skin infection" as a general term, but veterinarians differentiate problems based on their depth and distribution, as treatment methods vary.
Current international guidance (ISCAID) for canine skin infections emphasises cytology before antimicrobials and prioritises topical therapy for superficial diseases, reserving systemic antibiotics for deeper infections or when topical management is insufficient—an approach intended to improve outcomes and reduce pressure on antimicrobial resistance (Loeffler et al., 2025). ISCAID stands for the International Society for Companion Animal Infectious Diseases.
How is cellulitis diagnosed?
At The Andys Veterinary Clinic, an effective work-up typically includes:
History and physical exam

We assess the rate of progression, the level of pain, its impact on functionality, such as limping, as well as any recent grooming, encounters with fights, thorns, or field walks, and potential nail injuries, injections, surgeries, or dental issues.
Cytology (a fast, high-value test)

Skin cytology is a rapid method for identifying various elements, including bacteria and their morphology, inflammatory cells such as neutrophils, and assessing the likelihood of infection. It also helps determine whether empirical therapy is appropriate. The ISCAID guidelines strongly advocate for performing cytology before initiating antimicrobial treatment in cases of canine bacterial skin disease (Loeffler et al., 2025).
Culture and sensitivity testing (when indicated)

Bacterial culture may be recommended in several situations. This includes cases where the infection is deep, extensive, or recurrent, as well as instances in which prior antibiotics were recently used. Additionally, if there is a poor response to initial therapy or concerns about resistant organisms, bacterial culture may be warranted. This procedure is particularly important in chronic or recurrent infections caused by Staphylococcus pseudintermedius, where reports of resistant strains are becoming more common (Lynch, 2021).
Imaging (case-dependent)

Ultrasound machine Ultrasound can assist in locating an abscess pocket or a tract containing a foreign body. In cases involving the ocular or orbital regions, advanced imaging or a referral might be necessary, depending on the severity and suspected source of the issue (Hamor, 2024).
Treatment
Treatment is individualised based on severity, location, and diagnostics, but it typically includes several layers:
Address the source
The process involves clipping and cleaning the wounds, draining any abscesses if they are present, and removing any identified foreign bodies. Additionally, it is important to manage any underlying triggers such as allergies, ectoparasites, and self-trauma.
Pain control and supportive care
Cellulitis is painful. Comfort-focused care improves appetite, mobility, and recovery and reduces stress-related self-trauma.
Antimicrobial therapy (topical and/or systemic)
Topical antiseptics, such as those based on chlorhexidine, may be utilized as adjunctive treatments when feasible. Systemic antibiotics are often necessary for managing deep infections or cellulitis, and their use should ideally be guided by cytology and, when suitable, culture and susceptibility testing. International guidelines for treating canine pyoderma recommend a topical-first approach for superficial infections, while systemic therapy is advised for deeper infections. It is important to reassess the situation to ensure complete resolution and to prevent unnecessary prolongation of treatment (Loeffler et al., 2025). The guidance on veterinary pharmacology emphasizes that bite wound infections can involve organisms such as Pasteurella spp. (particularly significant in cats) and that the selection of antimicrobials should consider the likely pathogens and the clinical context.
Recheck examinations matter.
Deep infections may appear to improve on the surface, even when the deeper tissues remain inflamed. Follow-up examinations are essential to confirm that swelling and pain have genuinely resolved, that no foreign body or abscess is still present, and that the chosen antibiotics are still appropriate, particularly in cases of partial response.
Why does early treatment matter?

Untreated cellulitis in companion animals can result in several serious complications. One of the most common outcomes is the formation of abscesses, which are localised collections of pus that can cause significant pain and discomfort (Loeffler et al., 2025). Additionally, the condition may lead to tissue necrosis, wherein the affected tissues begin to die due to lack of blood flow or severe infection. This necrosis can further exacerbate the animal's condition and complicate treatment efforts. Furthermore, if the infection spreads into the bloodstream, it can result in sepsis, a life-threatening systemic response to infection that requires immediate medical intervention (Loeffler et al., 2025). In certain cases, particularly those involving the orbital region, cellulitis can also lead to vision loss due to orbital disease, which poses a significant risk to the animal's quality of life.
To mitigate these risks, prompt veterinary care is essential. The implementation of diagnostic measures such as cytology and culture, when indicated, allows for accurate identification of the causative agents. Furthermore, the use of targeted antibiotics significantly enhances treatment outcomes and reduces the likelihood of severe complications (Loeffler et al., 2025). Therefore, timely intervention is crucial in managing cellulitis effectively in companion animals.
How is Cellulitis Prevented?
Effective prevention measures include several important strategies. First, it's crucial to quickly clean and have any bites or scratches evaluated by a veterinarian. Consistently managing ticks and fleas is also essential to reduce scratching and protect the skin barrier. Regularly inspecting paws after walks is important since thorns and grass awns are common irritants. Additionally, addressing underlying itch or allergy issues early can greatly enhance overall skin health. Finally, proper grooming and coat care, especially for breeds with long coats, are vital in preventing skin problems.
A special note: “juvenile cellulitis” is different
Owners sometimes see “juvenile cellulitis” online. This is a distinct condition (often immune-mediated) seen in puppies and is not the same as bacterial cellulitis. It typically affects the face and lymph nodes and requires veterinary diagnosis and targeted therapy.
References
Bannoehr, J., & Guardabassi, L. (2012). Staphylococcus pseudintermedius in dogs and cats: An emerging zoonotic pathogen? Veterinary Microbiology, 157(1-2), 1-12.
Gelatt, K. N. (2018, reviewed/revised; modified Sept 2024). Disorders of the orbit in dogs. In Merck Veterinary Manual. Merck & Co., Inc. Retrieved January 6, 2026, from https://www.merckvetmanual.com/dog-owners/eye-disorders-of-dogs/disorders-of-the-orbit-in-dogs?utm_source=chatgpt.com
Haag, A. F., Fitzgerald, J. R., & Penadés, J. R. (2014). Staphylococcus aureus in animals. In F. M. Power (Ed.), Staphylococcus aureus (pp. 603-625). American Society for Microbiology.
Hamor, R. E. (2024). The orbit in animals. In MSD Veterinary Manual. Merck & Co., Inc. https://www.msdvetmanual.com/eye-diseases-and-disorders/ophthalmology/the-orbit-in-animals
Johnson, T. (2023, July 19). Cellulitis in dogs and cats. Veterinary Partner – VIN. https://veterinarypartner.vin.com/default.aspx?catId=102903&id=11604956&ind=613&objTypeID=1007&pid=19239&utm_source=chatgpt.com
Loeffler, A., et al. (2025). Antimicrobial use guidelines for canine pyoderma. International Society for Companion Animal Infectious Diseases (ISCAID).
Lynch, S. A. (2021). The complex diseases of Staphylococcus pseudintermedius in canines: Where to next? (Review article). PMC
Maggs, D. J., Miller, P. E., & Ofri, R. (2018). Slatter’s fundamentals of veterinary ophthalmology (6th ed.). Elsevier.
Miller, W. H., Griffin, C. E., & Campbell, K. L. (2013). Muller and Kirk’s small animal dermatology (7th ed.). Elsevier.
O'Shea, K. M., & Gray, B. M. (2016). Is the colonisation of Staphylococcus aureus in pets associated with human contact? Journal of Biomedical Science, 23(1), 41. doi.org
Roberts, E. (2024). Not just in man’s best friend: A review of Staphylococcus pseudintermedius host range and human zoonosis. ScienceDirect
Ruiz-Ripa, L., Abdullahi, M. G., Idelevich, E. A., & Hernandez, M. (2021). Nasal Staphylococcus aureus and S. pseudintermedius in healthy humans and dogs/cats: A meta-analysis. International Journal of Environmental Research and Public Health, 18(21), 11467. doi.org
Shipstone, M. (2025). Antibacterials for integumentary disease in animals. In Merck Veterinary Manual. Merck & Co., Inc. https://www.merckvetmanual.com/pharmacology/systemic-pharmacotherapeutics-of-the-integumentary-system/antibacterials-for-integumentary-disease-in-animals










Comments